Winning with Glycine part 2: is this simple amino acid the key to understanding and treating; diabetes, metabolic syndrome, obesity, and fatty liver disease?
In which we review glycine deficiency as both the consequence and cause of human metabolic disorders and how diet and supplementation is a simple, affordable, and effective therapy.
Introduction:
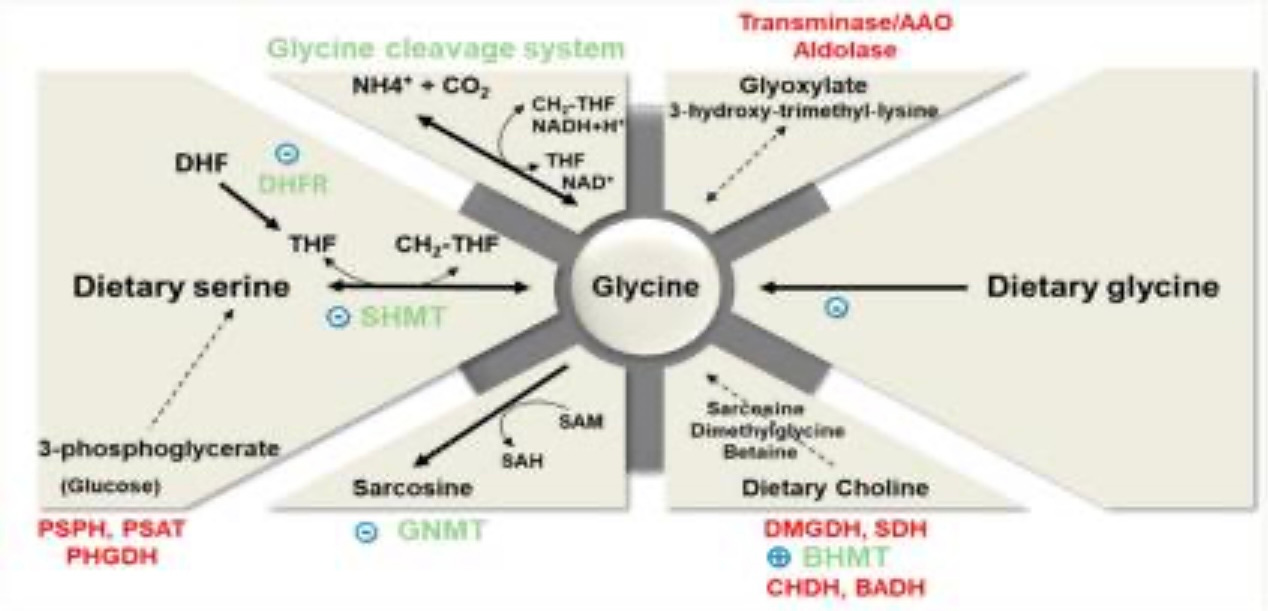
Happy New Year! In my first missive on glycine, I did a deep dive into the methylation cycle. The goal of part one was to provide an understanding of the biochemistry of methylation and how glycine fits in and what it does. I discussed that it serves as a buffer to the methylation cycle via its methylation into sarcosine which maintains a methyl group pool for later use. Then, I discussed how glycine is a valuable supplier of methyl groups to convert 5, 10 methylene tetrahydrofolate into the MTHFR substrate 5, methyl tetrahydrofolate using the glycine cleavage enzyme system. I also reviewed some of the basic functions and structures in the body that glycine is essential for, as well as its chemical structure. If you missed this article you can read it in my substack feed or by clicking this link HERE.
This article will be less about biochemistry and more about the practical application and real world scenarios. We will investigate the link between metabolic syndrome and glycine deficiency, and a surprising connection to glutathione deficiency. Then we will look at the impact of glycine supplementation and dietary intervention on these metabolic diseases. Lastly we will discuss how much glycine we should be getting from diet, why it’s preferable to consume collagen foods than relying on glycine powder. (I promise there will still be some biochemistry so don’t worry!) Without further ado, let’s dive in…
Part One: obesity, metabolic syndrome, and glycine deficiency are the epidemic of the modern age.
The connection between metabolic syndrome and glycine deficiency is well supported by the research, yet it is not widely discussed by doctors, nutritionists, or weight loss advocates. Even yours truly was not aware of it until I was doing research for my last glycine article and stumbled across it. The bottom line is that there is an inverse relationship between glycine levels and insulin resistance. This means the higher the fasting blood insulin and A1c, the lower the blood glycine levels.
What is metabolic syndrome?
Before we dive too deep into why this is the case, let’s review metabolic syndrome. The fact that it is called a syndrome, and not a disease is of huge significance to our discussion. A syndrome can be defined as a complex of symptoms without a clear cause or plan of treatment. Once the cause and treatment are known, then it is referred to as a disease. (1) Diabetes, for example, is a disease diagnosed by labs such as fasting blood glucose and A1C. If those labs are consistently too high then diabetes is diagnosed, and medications will be prescribed. The cause of the disease is understood to be out-of-control blood sugar and insufficient insulin to lower it so it can be called a disease and then treated with FDA-approved medications.
Metabolic syndrome on the other hand does not meet this criteria. Rather it is a complex of 6 symptoms that when 3 or more of them are observed, the patient is considered to have metabolic syndrome. Those symptoms are: high blood pressure, high total cholesterol, low HDL cholesterol, high triglycerides, high insulin levels, high blood sugar (but not too high so as to be diagnosed as diabetic), and lastly, too great of of waist circumference as a measure of obesity. Sometimes waist-to-hip ratio is used instead of simply measuring the waist circumference alone, which is how I was trained to assess a client. (2)
This is considered a syndrome because no clear cause for this constellation of symptoms is known or widely agreed on. (But we can certainly give a lot of the credit for modern epidemic to the processed food industry, sedentary lifestyles, and constant exposure to toxic chemicals) Furthermore, no clear FDA-approved medical treatment is available.
I am belaboring the distinction between disease and syndrome because it is so crucial to understanding why fully 1/3 of Americans and 1/4 of citizens of the United Kingdom and European Union are not being treated by the medical establishment for this condition. This is because it is not considered a disease-there is no cause and no treatment other than perhaps a pamphlet given about the topic and a stern talking to from the doctor about weight loss and exercise.
The consequences of metabolic syndrome, however, are widely understood and disastrous. Outside of chronic smoking and heavy drinking, untreated metabolic syndrome is the greatest risk factor for, and greatest predictor of, developing heart disease, type 2 diabetes, fatty liver disease, and some cancers. It affects perhaps as much as a billion people worldwide and is the principle driver of incalculable amounts of suffering and premature death. (2)
Part 2 The glycine connection:
Perhaps a 7th diagnostic criteria for metabolic syndrome could be reduced blood levels of glycine since this has been observed in recent research. More than just metabolic syndrome, reduced blood levels of glycine have been seen in diabetes, fatty liver disease, and obesity. Fahed et al in their 2019 review of clinical studies on this topic found that on average those with the conditions mentioned in the previous sentence have between 15-20% reduced blood glycine levels than healthy controls. Part of their review includes the famous Framingham Heart Study and the Malmo diet and cancer study, which between them have over 1800 participants. This is an important point as we aren’t looking at merely a tiny study with 10 participants but much greater sampling which gives us more confidence in the findings. Fahed et all also look at about 10 smaller studies as well, all with similar results which makes this a solid conclusion. Basically, to sum up their findings simply, patients with obesity and the resulting insulin resistance show reduced glycine levels around 20% less than healthy patients which has many consequences.
The average person eats between 1.5 and 3.2 grams of glycine per day. This holds true across all diets- vegetarian, vegan, and omnivorous (including meats and fish) I found this surprising, as I had assumed an omnivorous eater would consume more glycine than a vegan but in fact, they don’t because the percentage of glycine is pretty uniform in the protein of plants and muscle meats. The exception is rice which while having little protein, has twice as much glycine per gram of protein than any other food except collagen. High glycine protein sources are indeed found in the omnivorous diet, but most meat eaters don’t like these high collagen foods- namely skin, bones, tendons, and connective tissues. We do get some glycine from the fibers and connective tissue in meats, with again the cheapest cuts that take hours to braise, having the most compared to the tender, more expensive cuts. (2)
Glycine is not considered an essential amino acid (meaning one we can only get from diet) because humans can synthesize it- but its synthesis is greatly limited. The average person synthesizes roughly 3 grams per day from dietary serine, (another amino acid) dietary choline, (with which my readers should be very familiar), and glyoxalate from carbohydrate metabolism. (requires vitamin b6) Of these 3 grams, roughly 2.5 grams of this is from serine, which we get in the diet easily, but there is a catch; We can’t make more than 2.5 grams from serine, because for serine to be converted into glycine, it requires the enzyme SHMT, (serinehydroxymethyltransferase), which requires folate and b6, and the end result is one glycine molecule, and one 5,10, methylene tetrahydrofolate molecule. It always has to make both products, yet the body only needs so much 5,10 mthf, and once the body has enough of it, its production will be inhibited, AND glycine’s as well. So you can see that we simply can’t make more than 2.5 grams of glycine from dietary serine due to these biochemical limitations.
I believe this is the case because our ancestors ate 100% of any animal they hunted down, not wasting a single calorie. They ate up the skin, fried the ears, and made soups of the tendons, joints, feet, tail, and other connective tissues not to mention all the organ meats, which are the most nutritious part of the animal. Natural selection is all about sparing energy and since for millions of years we ate high collagen foods, we didn’t need to use much energy to produce more. This all changed in the last 150 years, with the advent of modern technologies for feeding, growing, refrigerating, and transporting meats, that made the muscle meats only our wealthiest ancestors could afford, available to almost everyone. This is even more true today, since low collagen foods are simpler and faster to cook, whereas high-collagen foods like oxtail soup, short ribs, or trotters take hours to braise and are not as convenient.
Most people need over 15 grams of glycine per day. A full third of the daily glycine turnover is used to make glutathione, our master antioxidant. It’s estimated we need 12-15 grams per-day to support our body’s collagen -ie skin, tendons, joints, etc. Clearly we are already in trouble. Then consider that bile acid requires glycine, the methylation system requires it as discussed in my last article, and neurotransmitters like GABA require it. You might remember from my creatine article that glycine is needed in its manufacture, and lastly, it’s needed as a conjugate in liver detoxification to excrete harmful substances. Yet we saw above that most people eat less than 3 grams and synthesize about 3 grams, averaging 6 grams or less-this is a problem.
Part 3. Glycine deficiency as a root cause of metabolic disease:
Guasch-Ferré et al found in their 2016 systematic and meta-analysis of the metabolomic indicators that predict developing type 2 diabetes and found glycine implicated heavily: (3)
Blood circulating levels of glycine are reduced in obesity. This is thought to be due to the inflammation that visceral fat causes reducing the ability of the gut to absorb dietary glycine along with reduced rate of synthesis by the liver.
Glycine has the most impact on insulin sensitivity of all the amino acids.
Glycine blood levels have an inverse relationship with insulin resistance and a positive relationship with insulin sensitivity. Simply state, the lower the blood glycine levels, the more likely insulin resistance is to develop
As a direct result of the above point, glycine blood levels also show an inverse relationship with those who are likeliest to develop type 2 diabetes. This means the lower the glycine levels in the blood, the higher the likelihood of developing diabetes.
Children born to diabetics also have lower circulating levels of blood glycine, suggesting an epigenetic effect that can span generations (yikes)
Improving insulin resistance through weight loss, exercise, or even diabetes medications like metformin, improved blood glycine levels. (very cool!) (3)
Further compounding the problem, glutathione levels are greatly reduced in type 2 diabetics, as much as 60% in some patients. (2) Keep in mind that glycine is needed for our bodies to synthesize glutathione (as well as cysteine) This is devastating, as without adequate glutathione, oxidative stress will run rampant, leading to more inflammation, which in turn is a root cause of more insulin resistance, hypertension, and hyperlipidemia. I will do a whole article on glutathione, and how to improve levels of it safely and cheaply. But source 4 concludes that this alone is a driver of metabolic disease. The reason why is glutathione protects mitochondria from damage by hydrogen peroxide which is made in every cell as part of normal metabolism. Without glutathione, the mitochondria of the cells are damaged by the hydrogen peroxide l and won’t work properly. Naturally this would be more damaging in the most metabolically active cells, such as those in the pancreas and liver that control insulin and cholesterol.
Tying it all together:
From this we can conclude that: obesity leads to reduced glycine absorption in the gut which leads to worsening insulin resistance which leads to lower levels of glutathione which leads to a gradual deterioration into diabetes and heart disease.
Part 4. The good news about reversing metabolic syndrome with diet and supplementation.
Now that we have laid out the problem, and perhaps thoroughly depressed you at the vicious cycle nature of metabolic syndrome and glycine deficiency, you might be wondering if there is any hope. The good news is that there is so much hope!
You might be thinking it stands to reason that since glycine deficiency is a culprit for developing insulin resistance then supplementing glycine or consuming collagen is going to be part of the answer and you would be 100% correct! Consider the following evidence:
Fahed et al note several studies in their systematic review that saw very positive results with glycine supplementation reversing insulin resistance in particular. (2)
A clinical trial found that 13-15 grams of collagen per day, ie two tablespoons of hydrolyzed collagen “Zhu et al. indicated that daily supplementation of 13 g of CPS(collagen powder) for 12 weeks led to a significant reduction in LDL, HDL, Triglycerides, total cholesterol, systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood sugar and HbA1c in patients with Type 2 diabetes mellitus and primary hypertension.”
Sekhar et al reported in their clinical trial that looked at 24 diabetics with severely reduced glutathione levels. This was corrected with glycine infusion and n-acetyl cysteine infusion which restored glutathione levels. (6)
These are just a few of many example of glycine or collagen supplementation improving all the markers of metabolic syndrome at the same time. The last one mentioned is of great interest since it shows glutathione levels being restored which is so crucial. This improvement is independent of weight loss and exercise which will also improve all the markers of course. I would never dream of reducing the treatment for metabolic syndrome down to only taking glycine and eating collagen. Rather it is one component of a strategy that should involve:
weight loss
Exercise
A diet free of processed foods which are inflammatory b I’ll be writing a lot about what I consider to be optimal weight loss approaches in a future article featuring the weight loss strategy I used personally to lose over 80 lbs and keep it off.
micronutrient support, such as with college, glycine, choline, b vitamins, high dose vitamin C, creatine
So it would be reductionistic and dangerous to say that taking glycine solves the problem with metabolic syndrome. However, as I have tried to show clearly above, glycine deficiency is part of the etiology of metabolic syndrome, and simply correcting this deficiency will begin to fix it and its a simple place to start, and get you feeling better right away. When you start to feel better it is so motivating to keep making health changes, and it helps a lot to have a simple goal such as taking collagen powder every day, as opposed to a huge goal such as losing 100lbs, and let the success of the small goal lead to taking bigger and bigger bites out of the huge goal.
Part 5: how to get more glycine every day
So how do we fix glycine deficiency? As I had said above, we need about 15 grams per day on average, those who eat a lot of animal protein will need more to balance out their methylation from the high methionine intake (see my glycine and methylation article for more info) Most people eat around 2-3 grams per day and can make another 2-3 on average and so you might think we need 10 grams extra per day, BUT those with metabolic syndrome or diabetes will both absorb less from food and make less than 3. (2) If you don’t have a metabolic condition then 10 grams should be fine but if you do then I recommend 15-20 grams per day. Let’s discuss how :
You can simply buy glycine powder and take up 15 grams per day, starting much lower and working up to that level over a few months. The upside of this approach is that glycine tastes ok, is affordable, and got positive results in many of the studies, so there is good evidence supporting its use.
One teaspoon is 3 grams, so 5 teaspoons per day will be 15 grams.
15 grams is the tolerable upper limit dosage and I don’t recommend taking more than this
I recommend spacing this out over 3 doses and taking with food to avoid nausea, which is a very common side effect.
Caveat: nausea, diarrhea, and other gastric issues are very common and you might not be able to tolerate it, which is why I recommend starting with 1 tsp (3 grams) and working up slowly over 2-3 months or taking collagen only.
2nd caveat-for some people glycine power stimulates the NMDA receptor, disturbing the glutamate/GABA balance and makes them feel terrible. I think this is because it causes the blood level to rise too fast. If this is your experience, stop immediately.
2. Take collagen powder. I think this is better choice than glycine powder for the following reasons:
easier on the stomach cause it is closer to food. It is still a processed product but is very easily absorbed
Won’t spike blood levels of glycine as much or as fast and is more likely to be tolerated by folks with the nmda receptor issue
Collagen has other amino acids, chiefly proline and hydroxyproline which have other benefits, especially for arthritis. We don’t have space to go into it here, but there we are many studies using supplemental collagen (not glycine) to help improve both pain joint mobility in osteoarthritis.
10 grams of collagen powder has about 3.5 grams of glycine. So to get 15 grams this way you need about 40-45 grams of collagen powder. This is probably impossible to consume in any other form but a smoothy which is how yours truly takes collagen.
Eat foods high in collagen.
1/2 ounce of pork rinds has 6 grams of collagen, giving you about 2 grams of glycine per serving. I eat at least this much every day.
Bone broth is a lousy source of collagen and glycine (7)
Sardines (if eaten whole) have about 5 grams of collagen per 150 grams of fish. Oxtails have about 3 grams per serving. If you eat chicken thigh with the skin you get about 3 grams of collagen per 100 grams of chicken.
There’s always room for jello! Jello is made from gelatin which is just another word for cooked collagen. A single 1/2 cup serving of jello contains as much as 5 grams of collagen! This is more likely to be one you make at home not a popular brand you see in the grocery store.
If you take magnesium (article coming soon on mag!) then take it as magnesium glycinate. It’s usually sold as 1000 mg of glycinate per 100 mg of magnesium. This is no different than glycine powder and has the same caveats as above.
Do all of the above! This is what I personally do. I take magnesium glycinate, always eat the skin of the chicken, eat pork rinds, and take collagen powder in a smoothy almost every day.
Conclusion:
Well this article went much longer than I intended, but I was so excited about the material that I didn’t want to leave any of it out and could’ve easily made it twice as long! I hope you are inspired to eat more collagen and take more glycine as another step on your health journey. As always, I am honored to be taking some of the steps with you and showing you the latest research.
All the best on your journey to better health!
Disclaimer: I am not a medical doctor or registered dietitian. The information in this article does not constitute medical advice and is not intended to diagnose or treat a disease, and is for educational and entertainment purposes only. Readers, especially those who are pregnant or lactating, should speak with their personal medical professional before acting on any of the information discussed.
references:
1. Calvo F, Karras BT, Phillips R, Kimball AM, Wolf F. Diagnoses, syndromes, and diseases: a knowledge representation problem. AMIA Annu Symp Proc. 2003;2003:802. PMID: 14728307; PMCID: PMC1480257.
Fahed G, Aoun L, Bou Zerdan M, Allam S, Bou Zerdan M, Bouferraa Y, Assi HI. Metabolic Syndrome: Updates on Pathophysiology and Management in 2021. Int J Mol Sci. 2022 Jan 12;23(2):786. doi: 10.3390/ijms23020786. PMID: 35054972; PMCID: PMC8775991.
Guasch-Ferré M, Hruby A, Toledo E, Clish CB, Martínez-González MA, Salas-Salvadó J, Hu FB. Metabolomics in Prediabetes and Diabetes: A Systematic Review and Meta-analysis. Diabetes Care. 2016 May;39(5):833-46. doi: 10.2337/dc15-2251. PMID: 27208380; PMCID: PMC4839172.
4. Hristov BD. The Role of Glutathione Metabolism in Chronic Illness Development and Its Potential Use as a Novel Therapeutic Target. Cureus. 2022 Sep 28;14(9):e29696. doi: 10.7759/cureus.29696. PMID: 36321012; PMCID: PMC9616098.
https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/effects-of-collagen-peptide-supplementation-on-cardiovascular-markers-a-systematic-review-and-metaanalysis-of-randomised-placebocontrolled-trials/D1BD51038B71D9A9BCA7880B1F6649F0#r22)
Sekhar RV, McKay SV, Patel SG, Guthikonda AP, Reddy VT, Balasubramanyam A, Jahoor F. Glutathione synthesis is diminished in patients with uncontrolled diabetes and restored by dietary supplementation with cysteine and glycine. Diabetes Care. 2011 Jan;34(1):162-7. doi: 10.2337/dc10-1006. Epub 2010 Oct 7. PMID: 20929994; PMCID: PMC3005481.
Alcock RD, Shaw GC, Burke LM. Bone Broth Unlikely to Provide Reliable Concentrations of Collagen Precursors Compared With Supplemental Sources of Collagen Used in Collagen Research. Int J Sport Nutr Exerc Metab. 2019 May 1;29(3):265-272. doi: 10.1123/ijsnem.2018-0139. Epub 2018 Sep 26. PMID: 29893587.



Great article, thank you!
Part 1? Looked in posts and did not find.