Glutathione part 1. The missing link in understanding the metabolic syndrome global pandemic
A deep dive post into this tiny yet crucial molecule that is the lynchpin of the antioxidant defense system and why its deficiency causes, and is caused by, metabolic syndrome.
Introduction:
In my last article, we looked at the intersection of glycine as both part of the etiology and treatment of metabolic syndrome and other metabolic disease states. If you missed that article you can read it HERE. You might also recall that I had discussed that endogenous glutathione production is reduced by as much as 60% in those with diabetes compared to someone without this condition, and glycine levels were also reduced. This was found to be a major factor in the etiology of metabolic disease, as the cells most affected by the lack of glutathione are highly metabolically active, such as the pancreas, liver, and brain, and are therefore the most prone to damage in the glutathione deficient state. What I didn’t explain is why this is the case. To answer that question, which is vitally important to living a long and healthy life, we need to understand the antioxidant defense system, and how glutathione is the keystone supporting that entire system. Then we will look at how glutathione deficiency leads to metabolic syndrome through the malfunctioning of the antioxidant defense system. This is a two-part article, as my amazingly beautiful, and brilliantly talented editor (my wife), mentioned my article was too long, almost 4000 words, and no one would hang in there for such long-windedness. So I have broken it up into two parts. Part two is 95% written but needs revision and will be released on Thursday of this week. It will cover a new test that diagnoses glutathione deficiency and metabolic syndrome and confirms this relationship. It will also look at the evidence showing that correcting glutathione deficiency reverses the symptoms of metabolic disease, and how to correct this deficiency. Today’s article will lay the foundation and the information is vital to understanding how to reverse metabolic syndrome, even if it does leave you on a bit of a cliffhanger.
Part One: What is glutathione?
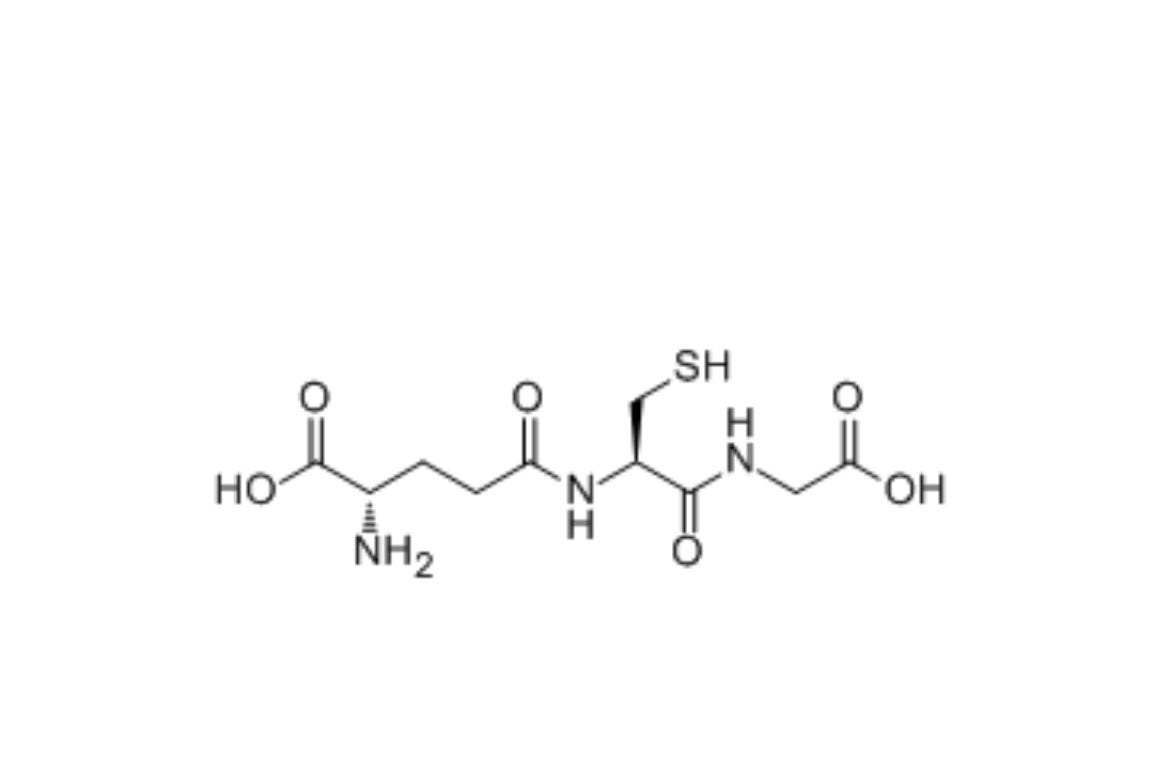
Glutathione is the most abundant sulfur-containing molecule in the human body that isn’t a protein. Rather it is a tripeptide, meaning that 3 amino acids have been fused together to synthesize a new compound. Those amino acids are glutamate, the most abundant amino acid in our body (and diet), glycine, and cysteine (pronounced sis-teen). In the molecule diagram above you can see sulfur indicated by the ‘SH’ which is known as a sulfhydryl group. Cysteine is considered a conditionally essential amino acid, meaning while humans can synthesize it, we can’t do so fast enough to meet demand and also need to consume it. Cysteine is the rate-limiting component of glutathione synthesis, meaning the synthesis of glutathione is limited by the availability of cysteine.
Some of the functions of glutathione are:
an antioxidant protecting almost every cell from destruction by oxidative stress
a regulator of the other antioxidants such as vitamin C, vitamin E, and vitamin A
a detoxifier of harmful chemicals
A neurotransmitter and protector of the brain
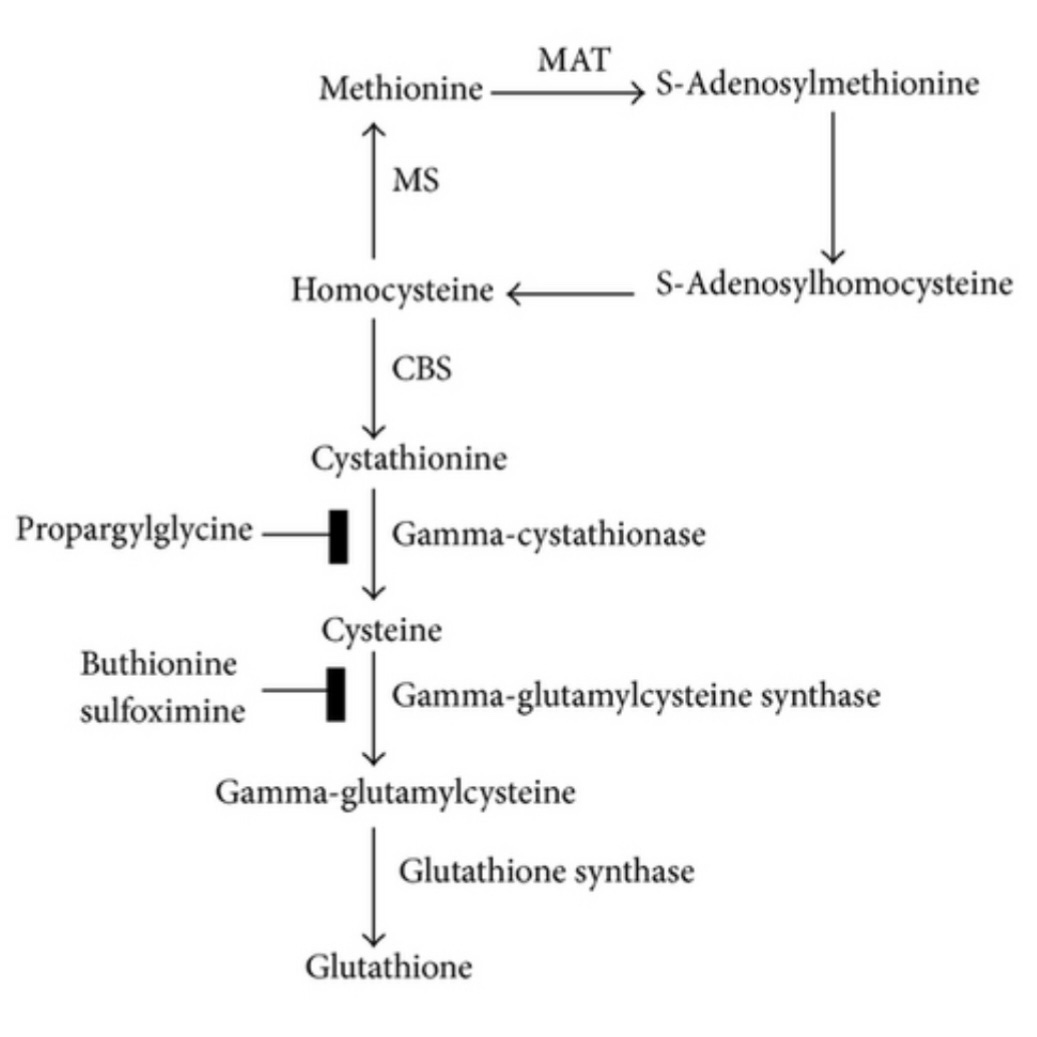
The diagram below shows the methylation cycle very briefly with homocysteine going up through the MTHFR and BHMT enzymes to form Methionine, which is then converted to S-adenosylmethionine, also known as SAMe, which is the end result of the methylation cycle. However, homocysteine can also go down into the transsulfuration pathway which will transform it into cysteine. While we do get some cysteine from diet, it is the transsulfuration pathway that our cells rely on for having enough on hand to make adequate glutathione. The transsulfuration pathway is initiated via the enzyme cystathionine beta-synthase(CBS). This enzyme converts homocysteine into cystathione, which in turn is acted on by gamma-cystathionase which converts it to cysteine. Cysteine can then enter the gamma-glutamyl cycle that combines it with glutamate and glycine, resulting in glutathione via a system of enzymes. The CBS enzyme and the transsulfuration pathway are activated when the cell detects rising levels of oxidative stress and the need for more glutathione to combat it. Something to consider is that CBS enzyme SNPs are very common, they slow down the rate of cysteine synthesis leading to low cellular glutathione and to high homocysteine. This is independent of SNPs on MTHFR which also leads to high homocysteine-a heart disease risk factor and is not something to ignore.
Part 2. The antioxidant defense system protects the mitochondria from oxidative stress and damage. Glutathione is the star player.
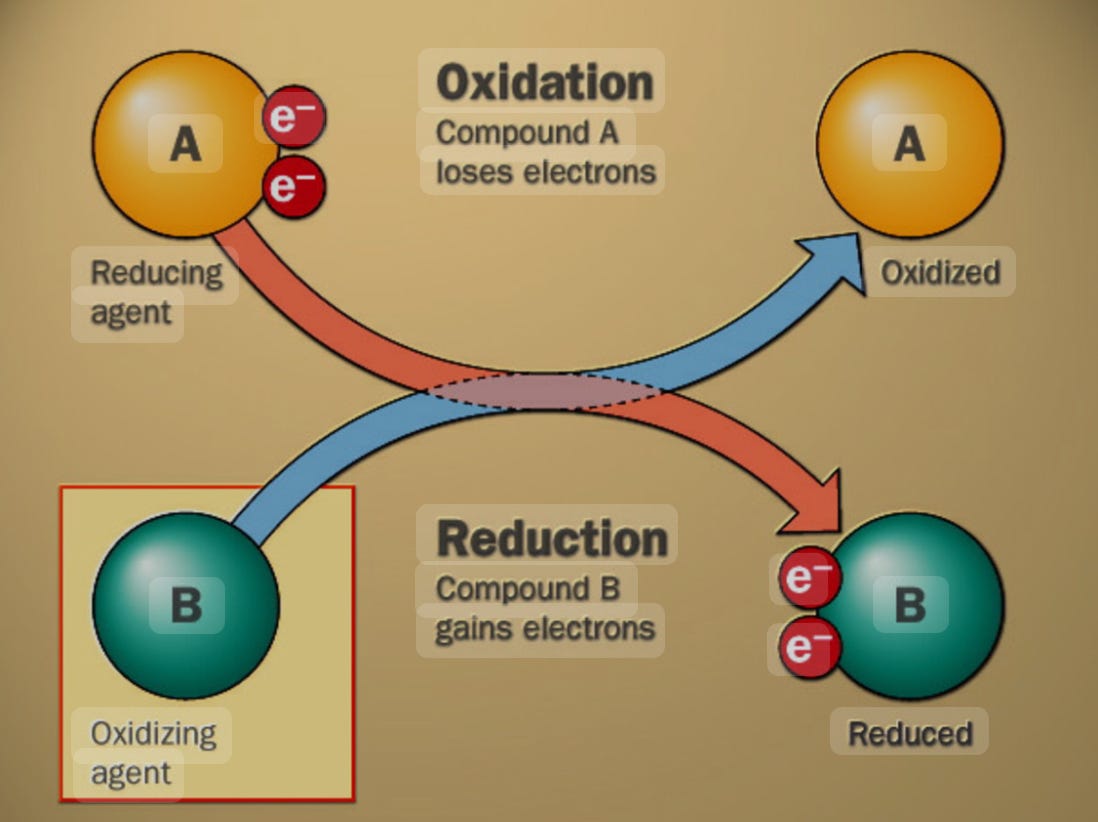
Consider the image above. You can see the two sides of what is called a redox reaction -so called because it consists of reduction and oxidation. Oxidation occurs when a compound loses one or more electrons. We now say this compound is in an oxidized state. When it encounters what is called a reducing agent, such as vitamin C, vitamin A, or vitamin E, just to name a few examples, then it takes the electrons from the reducing agent. Having had its missing electrons restored it is now in a reduced state and ready to donate its electrons yet again to another oxidizing agent. If there is no reducing agent, also called an antioxidant, then the highly reactive oxidating agent will steal electrons from other parts of the cell, usually the mitochondria, damaging it so it can’t function properly. This is called oxidative stress and it underlies the etiology of many disease states.
Our cells are actually making these oxidizing agents, day and night, almost unceasingly. They are called reactive oxygen species or ROS. This is due to the generation of ATP by the mitochondria which produce a strong ROS called superoxide. (O-) Superoxide is so toxic to the cells that our mitochondria have evolved an enzyme called superoxide dismutase for the purpose of converting superoxide into a compound you may have under your sink-hydrogen peroxide. (H2O2) Hydrogen peroxide, while less toxic than superoxide is still quite toxic to cells, which is why it works so well as a topical disinfectant- it kills bacterial cells on contact by submitting them to severe oxidative stress and they die.
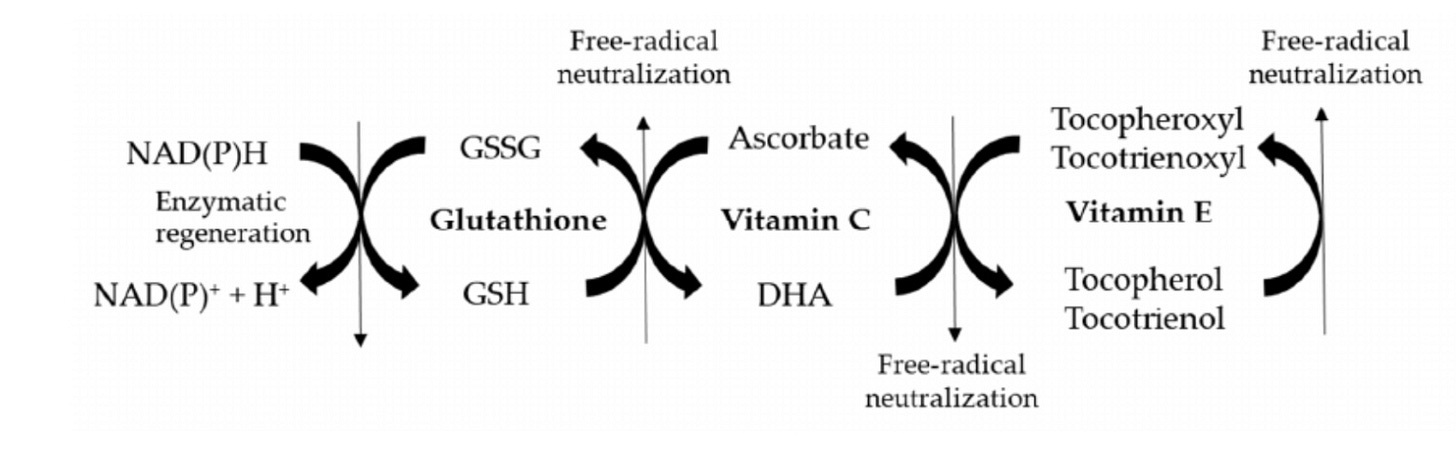
To protect our mitochondria and cells from a similar fate, the antioxidant defense system rushes to the rescue! This is where glutathione, acting as a superhero donates its electrons to the hydrogen peroxide molecule and reduces it from toxic H2O2 into two molecules of harmless H2O(facilitated by an enzyme called catalase). But now, glutathione has lost its electrons and is now in the oxidized state and needs to be regenerated. To glutathione’s aid leaps another superhero, NADPH, which is a niacin-derived (vitamin B3) molecule that the body makes as part of glycolysis using the pentose phosphate pathway (much more on this in later articles). NADPH donates its electrons to glutathione and it is now reduced and ready to save the cell from the next wave of hydrogen peroxide. Vitamin C also both regenerates and is regenerated by glutathione.
Take a look at the chart below to see the chain of antioxidants working together. Vitamin E’s unique role is to reduce free radicals formed from fats and oils. When it does so, it can ONLY be recycled by vitamin C, which in turn requires glutathione to be rejuvenated. Glutathione then is reduced by NADPH.
From this, you can see how crucial it is to not be deficient in any of these compounds, but glutathione and vitamin C are the true stars in this show, requiring constant synthesis in the case of glutathione, and constant intake of vitamins C and E, since humans are unable to synthesize them. You can also see how these nutrients are interlocked and interrelated. If you are deficient in any one of them your cells will undergo oxidative stress with terrible downstream consequences.
Part three. Lack of glutathione and the corresponding oxidative stress set the stage for modern chronic disease.
Glutathione deficit is both caused by and is also a cause of metabolic disease. Consider this quote from Hristov et al:
without adequate GSH (glutathione)... oxidative stress is most pronounced in metabolically stressed cells, and the accelerated damage to these organelles can lead to premature dysfunction and early cell senescence, culminating in cell death [24]. Thus, in the most metabolically active tissues such as renal cells, hepatocytes, endocrine cells, endothelial cells, and neurons, low GSH levels should be expected to be directly correlated with worse cellular function and early cell death. (1)
Let’s break this down: As we covered above, the mitochondria are constantly cranking out reactive oxygen species as part of normal energy metabolism. Without glutathione (and the other antioxidants also), oxidative stress damages the cell, leading to dysfunction, senescence (loss of the ability to divide and grow), and cell death. The cells implicated are the most metabolically active, which makes good sense to me, as they will be the ones producing the most ROS and most likely to burn through limited supplies of antioxidant nutrients. You will notice that each of the cells mentioned are those whose dysfunction ties into a feature of metabolic disease:
Hepatocytes: (liver cells) When these don’t function as well, high cholesterol and fatty liver disease are the result
Most of the body’s glutathione is made in the liver, and the body will make much less when the hepatocytes are disturbed. This is one way that metabolic syndrome is both caused by and causes low glutathione.
endocrine cells: (pancreas) Damage to the pancreas is the precursor to insulin resistance which causes metabolic syndrome and diabetes.
endothelial cells: (blood vessels) This is where we see high blood pressure, arteriosclerosis, and atherosclerosis.
renal cells: (kidneys) This is evidenced by low GFR scores indicating kidney damage and kidney disease.
neuronal cells: (brain and nervous system) this leads to diabetic neuropathy and brain disorders.
You might remember from my last article, that metabolic syndrome is defined as having 3 out of 6 conditions: high blood pressure, insulin resistance, high total cholesterol, low HDL cholesterol, high triglycerides, and high hip-to-waist ratio. Hristov makes a strong case that low glutathione levels are implicated in these symptoms. I focused on low glycine blood levels and showed how correcting them through dietary collagen and glycine could reverse these symptoms and should be part of a comprehensive therapeutic approach to treating metabolic disease. I also briefly hinted at the perhaps broader truth, which is that much of the benefits of this treatment came from the fact that increasing blood levels of glycine caused glutathione levels to rise. This is because glycine is one of the precursors to glutathione synthesis, and we will make less of it, when glycine levels are chronically low, as is the case for most people eating a modern diet of processed food.
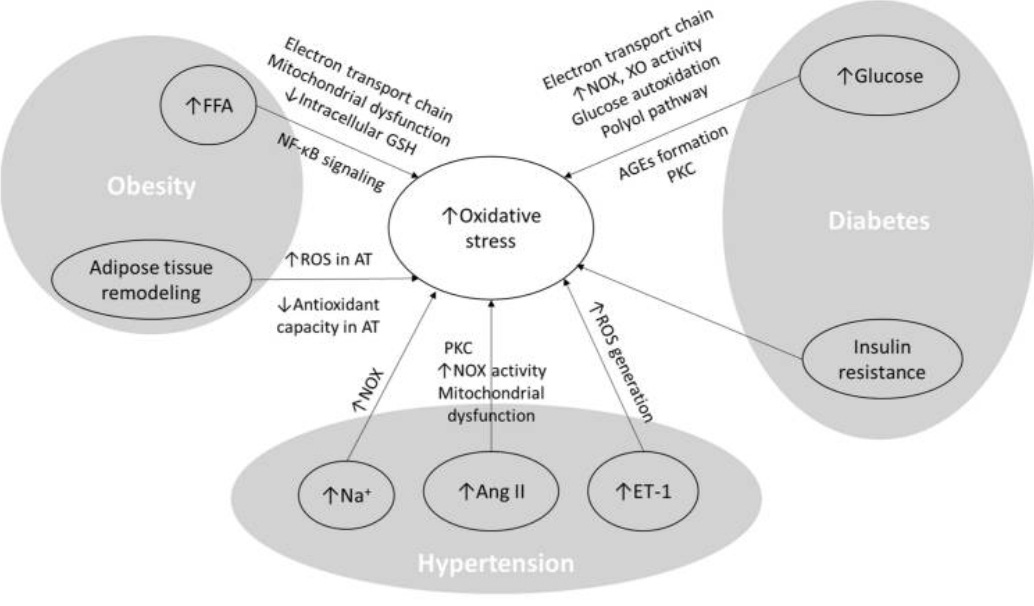
Sharebiani et al, in their 2024 review and meta-analysis conclude the following: “All components of MetS(metabolic syndrome), including obesity, adipose tissue remodeling and dyslipidemia, hyperglycemia, insulin resistance and hyperinsulinemia, and hypertension, participate in the production of oxidants and the activation of oxidative stress pathways” (3)
The graphic below ties this all together. On the right, we see elevated glucose and insulin resistance forming AGEs (much more to say about this later, but for now these are inflammatory sugar-protein measured by the A1C test) that causes oxidative stress. On the bottom we see hypertension leading to increased ROS generation, increased NOX (nitric oxide) activity, and more oxidative stress. Obesity leads to nf-kB signaling (more in other articles), mitochondrial dysfunction, and reduced intracellular GSH, which is the shorthand for glutathione. Lastly, adipose tissue remodeling leads to increased ROS, and decreased antioxidant capacity. All this leads to more oxidative stress, and fewer antioxidants to fight it, especially considering the vitamin C, E, and A deficient, standard American diet. A vicious cycle is generated, that leads to progressively worsening disease states, which is why if no action is taken, metabolic syndrome becomes diabetes, heart disease, cancer, and increased all-cause mortality. Remember that 1/3 of Americans and the British have metabolic syndrome, and 1/4 of Europeans, and the numbers are rising rapidly in Asia, Africa, and South America as well, as the Western lifestyle and diet spreads around the world. In my last article, I estimated over a billion people are affected.
Now that I’ve given you the bad news, I am here to say there is hope! I believe anyone and everyone can reverse metabolic syndrome with proper information and motivation. Thursday’s article will look at how diets low in vitamin C (extremely common, the vast majority of people’s diets) lead to glutathione deficiency and how this is so easy to reverse. We will look at new research on the GGT test which very accurately diagnoses low intracellular glutathione as seen in the graphic above and metabolic syndrome as well, and is a strong predictor of developing heart disease. Lastly, it will look at some potent nutritional strategies I have implemented for myself and my clients to reverse glutathione deficiency and the symptoms of metabolic syndrome. Stay tuned!
* I have almost 1000 subscribers. My goal when I started this newsletter service was to get to 1000, and then turn on paid subscriptions and offer extra services for paying members. Probably a Q&A thread where I members can submit questions and get more personalized answers. But if you have any ideas of what you would consider a nice perk for $5 per month I am open to ideas! Please comment or send me a DM with any ideas of what services you would find valuable. This is all new to me and your feedback and suggestions would be greatly appreciated! I will always keep my core articles free as I want this information to be available to everyone, anywhere in the world, free of charge. Thank you so much for reading, subscribing, and telling your friends.
All the best on your journey to better health!
Disclaimer: I am not a medical doctor or registered dietitian. The information in this article does not constitute medical advice and is not intended to diagnose or treat a disease; it is for educational and entertainment purposes only. Readers, especially those who are pregnant or lactating, should speak with their personal medical professional before acting on any of the information discussed.
References:
Hristov BD. The Role of Glutathione Metabolism in Chronic Illness Development and Its Potential Use as a Novel Therapeutic Target. Cureus. 2022 Sep 28;14(9):e29696. doi: 10.7759/cureus.29696. PMID: 36321012; PMCID: PMC9616098.
Forman HJ, Zhang H, Rinna A. Glutathione: overview of its protective roles, measurement, and biosynthesis. Mol Aspects Med. 2009 Feb-Apr;30(1-2):1-12. doi: 10.1016/j.mam.2008.08.006. Epub 2008 Aug 30. PMID: 18796312; PMCID: PMC2696075.
Sharebiani H, Mokaram M, Mirghani M, Fazeli B, Stanek A. The Effects of Antioxidant Supplementation on the Pathologic Mechanisms of Metabolic Syndrome and Cardiovascular Disease Development. Nutrients. 2024 May 27;16(11):1641. doi: 10.3390/nu16111641. PMID: 38892574; PMCID: PMC11175159.


Thank you. I appreciate you keeping your costs low. If I had to pay for all the great information out there, I would be broke.
Thanks for posting